
In our experience, the epithelium-on (epi-on) procedure allows patients to experience faster, more comfortable recovery while also reducing the risk of infection and scarring. Although removing the epithelium allows faster penetration of riboflavin into the corneal stroma, in our practice we have seen that it may also result in longer healing time (especially in a diseased cornea), an increase in postoperative pain, and higher risks of scarring and infection. Is it better to leave the epithelium intact or remove it for CXL? The only FDA approved device for CXL is labeled for epi-off CXL. Notice the crab-claw appearance indicating pellucid marginal degeneration in the keratometric images (B). This grading scale is helpful when classifying a new keratoconus patient or monitoring an existing patient. TKC gives a grading from 0 (normal) to 4 (severe). Topographical keratoconus classification (TKC) value (in red, bottom of center column) = KC3 (A). Pentacam images showing pellucid marginal degeneration. We expect the likelihood of future corneal transplants to be greatly reduced for patients with keratoconus due to early intervention with CXL.įigure 2. In our practice we have treated patients as young as 12 years and successfully halted the progression of keratoconus before it affected their vision. By halting the progression of keratoconus early, we give patients their best chance for maintaining the best visual potential. We recommend CXL to patients as early as possible in the progression of keratoconus (Figure 1). In 2016, the FDA approved the KXL System and Photrexa riboflavin formulations (Avedro acquired by Glaukos in 2019) for performing epithelium-off (epi-off) CXL procedures. 2 We’ve seen the benefits of CXL in strengthening the cornea, flattening keratometric values, and improving UCVA and BCVA. Twenty years ago, corneal collagen crosslinking (CXL) techniques were developed by researchers at the University of Dresden. Transplant options now include deep anterior lamellar keratoplasty (DALK) and penetrating keratoplasty (PKP). If the cornea becomes too thin or severely scarred, however, such as in the advanced stages of keratoconus, a corneal transplant may be the best treatment. Some mild stage keratoconus patients can be successfully managed by correcting distortions in vision with spectacles or specialty contact lenses. CXL can be a comanaged procedure if the comanaging doctors are comfortable with the arrangement.Epithelium-on CXL can be easier on patients, with faster recovery and less risk of infection.Only epithelium-off CXL is approved for use by the FDA.During your examination, you will learn about your candidacy for scleral lenses, including an estimate of out-of-pocket costs. To learn more about your keratoconus, call ReVision Optometry today to schedule your examination at 619.299.6064 or request an appointment online. These days, scleral contact lenses are a common and effective treatment for keratoconus, including if your eye doctor diagnosed PMD. The treatment to restore vision is the same if you have PMD or classic keratoconus: specialty contact lenses with a rigid surface are the gold standard for visual rehabilitation. If your doctor told you that you have PMD, you likely get decent vision with updated eyeglasses and received diagnosis later in life compared to others with keratoconus. PMD is the same thing as keratoconus, just a subclass of it. The fact that some patients have a PMD-type topography in one eye and a more classic keratoconus topography in their other eye, also supports that these are the same disease entity. In other words, most patients with PMD likely had onset of their corneal distortion in the adolescent years despite diagnosis coming much later due to mild symptoms. Since many patients with PMD achieve good vision with eyeglasses with the bulk of the corneal distortion decentered downward out of the line of sight, PMD would often get diagnosed later because vision symptoms often are more subtle. Many eye doctors and patients incorrectly assumed that the time of diagnosis was also the time of onset. But in fact, PMD is often diagnosed later because it tends to impact vision less. Second, PMD supposedly had a later onset in life.
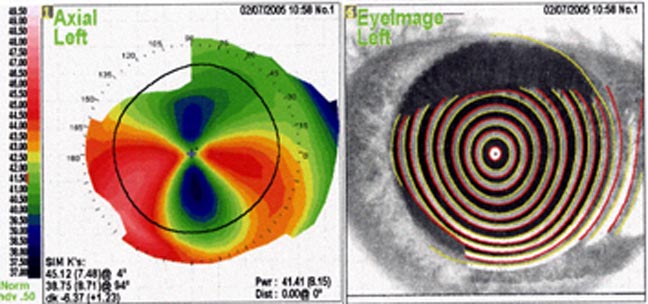
Reprocessing an axial topography to tangential view generally uncovers a classic keratoconus pattern for most alleged cases of PMD (Figure 2). A topography can be viewed as an “axial map” which smooths out data points, or as a “tangential” map which provides a more point-to-point assessment of light bending power. First, the classic “crab-claw” or “butterfly” topography pattern attributed to PMD (Figure 1) was just due to the way the topographical map was viewed. Two factors previously confused eye doctors into believing that PMD and keratoconus were separate eye conditions. Same topography as Figure 1 but under a tangential view.


 0 kommentar(er)
0 kommentar(er)
